Out of the Mouth of Infants and Nursing Babies

Nursing care of the newborn patient requires additional skills and knowledge for the nurse to efficiently accost the needs of these patients. Textbooks ascertain the newborn phase as lasting from anywhere between the moment of birth until the first four weeks of life, or 28 days after commitment.
While most deliveries are considered a routine procedure (either via NSD or Caesarian section), some newborns may present with risk factors and other symptoms that require immediate intervention. Because of this, the nurse who is responsible for the care of newborns should be knowledgeable about how to manage these patients as they transition from intrauterine to extrauterine life.
The American Academy of Pediatrics and the American Congress of Obstetricians and Gynecologists have included in their guidelines several levels of care that involve the neonate. These levels are:
- Level 1- or bones neonatal care, involves the meeting of minimum requirements by any facility that performs birthing services. These include having the essential trained personnel and equipment to perform neonatal resuscitation and stabilization. They should also take the capacity to coordinate referrals for newborns needing more specialized care.
- Level Two- are birthing facilities that are reserved for newborns who have been stabilized and are moderately ill, born on or a few weeks over 32 weeks of gestation. They may weigh a little more than than 1500 grams at birth and may demand to be immediately transported to specialized facilities urgently. While nearly of these newborns may exist delivered nether uncomplicated conditions, their weights and ages of gestation may point a need for more specialized care.
- Level III- are facilities that cater to caring for infants born at less than 32 weeks of gestation, and are ordinarily categorized every bit pre-term. These facilities should have practitioners who have training and experience in providing neonatal life support, physiologic monitoring, imaging, and diet. Nurses who are assigned at these facilities should also have the skills to provide psychosocial intendance to the family of the infants.
- Level IV- are facilities that are capable of providing highly specialized care to patients with critical conditions equally well every bit those who need firsthand ambitious therapy for circuitous conditions such as congenital cardiac malformations, spinal cord anomalies, and other life-threatening atmospheric condition.
Nurses who are caring for neonates, regardless of the level of intendance required, should have the necessary preparation to treat infants. These requirements include neonatal resuscitation certification and training, which must be renewed every ii years. Furthermore, other skills related to postpartum care and newborn resuscitation should be updated, such as:
- Temperature monitoring and command
- Pulse oximetry monitoring
- Provision of intendance for the infant under warmers/warming equipment
- Caring for infants with orogastric tubes and IV lines
- Monitoring infants under isolettes or incubators
There are several indicators of a newborn'due south wellbeing that the nurse needs to have into consideration when assessing these patients and planning for care. First among these is the APGAR Score.
What is the APGAR Score?
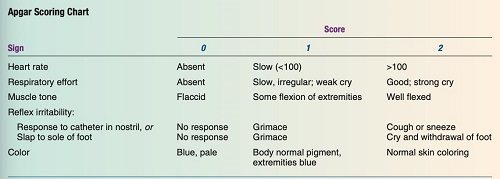
The APGAR Score is an acronym that denotes specific areas of assessment that must be evaluated between the starting time and fifth minutes of life. Individual parameters are scored. The highest possible score for each of the five areas is two, while the lowest possible score is 0. The following is how scoring is interpreted:
- 0-three points: the score indicates that the child may be in danger; immediate resuscitation is needed; the kid may need to be transferred to an urgent care facility
- 4 – 6 points: the assessment may indicate potential airway or breathing bug, and at that place is a need for oxygen supplementation
- vii-10 points: a favorable finding and unremarkably indicates that the babe is in good health.
The APGAR Score follows the table below in the assessment of the newborn. Note that assessments are washed immediately afterwards nativity (first minute of life) and v minutes later to serve equally baseline data and indicate the infant's adjustment to extrauterine life. Findings are documented, and any indicators that need immediate attention are reported to the medico for immediate attending.
Assessing for General Baby Wellbeing
The most critical menstruum immediately post-obit the infant's birth is between the showtime few minutes and at to the lowest degree the starting time 8 hours of life. This is due to the neonate gradually transitioning and adjusting from life inside the uterus to life outside the uterus. The lungs, which the placenta had previously oxygenated, are now being oxygenated as the infant breathes.
Apart from this pregnant adjustment, the infant is also suddenly exposed to colder temperatures outside the warm environment of the uterus, and his connexion to his mother'due south nutrient flow via the umbilical cord is cut. Therefore, the nurse needs to conduct a thorough cess to determine priority nursing care, rule out potential bug, and ensure that the neonate'southward transition to extrauterine life will go as smoothly as possible.
A. Respiratory Cess
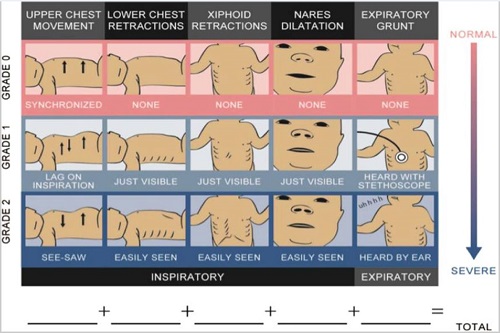
Considered to be one of the top priorities in caring for the newborn, assessing the infant's respiratory condition goes beyond the APGAR scoring. Immediate evaluation of respiration is performed using the Silverman and Andersen Index, which evaluates the infant using five criteria:
- Chest movements- should exist symmetrical during respiration; spontaneous; asymmetrical movements are scored 1 or two depending on the severity
- Intercostal retractions- should not be present (score of 0)
- Xiphoid retractions
- Dilation of the nares during respirations- indicative of the difficulty in breathing (infants are obligatory olfactory organ breathers)
- Expiratory grunting- may indicate airway patency problems.
While the highest score for APGAR is betwixt 7-10 and indicates good fetal well-being, the Silverman and Andersen Index scoring is the opposite. A score of 0 indicates that the fetus is not experiencing any respiratory distress, while a score between 7-10 indicates severe respiratory distress. (see figures below)
B. Physical Exam
A thorough physical exam is performed on the infant to place any observable conditions or concrete deformities that may necessitate immediate intervention or referral to a more specialized facility. When assessing the newborn physically, keep the post-obit points in listen:
- Cess should be done quickly to avert overexposing the newborn
- Respiratory assessment should be the start to be washed
- Make up one's mind the height (in cm) and weight of the infant as this helps determine maturity compared to average ranges for age of gestation.
- When weighing newborn, ensure that this is done at the same time each twenty-four hours to help note for any abnormal weight losses or gains
- Blood testing may exist required to exist performed such as the heel-stick exam to determine blood glucose, hemoglobin, hematocrit, bilirubin and other parameters
- Behavioral capacity assessment for the newborn may also be done to help determine ability of the baby to interact with the people effectually them.
C. Immediate Care of the Newborn Upon Birth
Ideally, the newborn receives immediate intendance in a separate area from his mother in the birthing suite/facility. This expanse is typically equipped with a heated table, warming blankets or other related equipment, a resuscitation set, eye ointment, suction equipment, and other relevant materials. In order to provide immediate care for the newborn, the following actions are taken:
- Placing an identification band around the newborn's arm or leg and creating his own registry. This aids in the identification of the newborn and the prevention of infant switching.
- Footprints of the newborn are taken and kept for identification. In some cases, additional copies may exist given to parents/families who asking to accept it.
- Recording of the name of the babe in his EMR. If the infant does not accept a proper noun nonetheless, he/she may be referred as Infant Boy/Girl (last name of mother/parents).
- Recording of APGAR Score, Silverman and Anderson Sore, birth weight, length and other anthropometric measurements, vital signs.
- Provision of immediate intendance such equally immunizations, bathing, swaddling, placement under bili-light/warmer and postural drainage.
- Feedings may be given to the infant depending on preference of the parents. Breastfed infants to feed immediately when the mother is able. Bottle fed infants are commonly fed later on ii-four hours upon delivery.
- Rooming-in of the babe with the mother is highly encouraged after vi-8 hours to promote bonding.
Other Expected Newborn Assessment Findings
Apart from assessing vital signs, caring for the newborn immediately later birth, the nurse also needs to have note of the post-obit cess findings that may be present among the newborn patients. While some of these findings are expected and may render to normal a few days after nascence, some may demand to be reported to the md for further evaluation and direction.
A. Head
- The baby'due south head is roughly i-4th the length of the entire body, and the sutures are still palpable. Sutures are expected to be completed in vi and 18 months, respectively.
- Due to passage through the birth canal, head molding may still be present. Information technology should not, withal, be widened. Molding is expected to subside 72 hours after birth.
- Birth trauma masses may also be present and are expected to go away in a few days:
- Caput succedaneum is an edema of the soft tissues that extends over the bone and crosses suture lines.
- Cephalhematoma- a type of swelling that is caused by bleeding into an area between the i and the periosteum. However, this bleeding does not cross over suture lines and is reabsorbed into the torso over a half dozen-week flow.
- Head lag is a common finding when pulling the newborn to a sitting position at least 3 months of age. The infant is expected to exist able to lift the head slightly and plow the head side to side when placed on a decumbent position
-
- The spine of the baby should appear to be directly, while the posture is slightly flexed.
- Movements should exist well-coordinated and sporadic. Hypotonic or hypertonic movements may indicate possible central nervous system impairment.
- No hair tufts or depression should be seen along the spinal column. Presence of these findings may indicate spina bifida or a possible opening of the spinal cavalcade.
- Extremities should accept a symmetrical and full range of motility.
- Fists of the babe unremarkably are clenched, with all 10 fingers separating and fanning out when the palms are open.
- Legs appear to be bowed initially and corrects over the first few years of life.
- Gluteal folds are even.
- Creases are nowadays along the soles of the feet and pulses are palpable in the brachial, radial and femoral sites. B. Optics
- The eyes should be clear and symmetrical.
- (+) PERRLA
- Glimmer reflex should be assessed and nowadays.
- The infant may appear to exist initially cross-eyed due to weak extraocular muscles. This will resolve over time.
- Red eye reflex is also present, and the baby is also able to runway and prepare his eyes on an object momentarily.
- Immediately after birth, the eyelids may appear to be slightly edematous due to the pressure on the baby's face during the birthing process. This may also exist due to the effects of the heart ointment practical in the immediate care later on delivery.
C. Ears
- The ears should exist symmetrical, cartilage is house and recoils
- The acme of the pinna should be on or higher up the imaginary line fatigued from the outer canthus of the optics.
- Note that low-fix ears may be indicative of a renal problem, Down syndrome or other genetic abnormalities.
D. Nose
- The nose may exist flat or broad and infants are obligatory nose breathers.
- Some infants may occasionally sneeze to remove whatever obstructions in the nasal passages.
- Nares should not flare and must exist patent at all times. Flaring nares may indicate respiratory distress.
E. Mouth
- Oral mucosa should announced pinkish and moist, with both hard and soft palates intact.
- Presence of Epstein'south pearls may be seen on hard palate. These are tiny white cysts and disappear over fourth dimension.
- The uvula should be positioned in the midline of the mouth, the tongue moving freely and has a brusk frenulum.
- Rooting and gag reflex should be present and the infant should present with a proficient sucking and swallowing reflex.
F. Cervix
- The neck should be able to hold the head in the midline position and is short and thick in advent.
- In that location should exist a expert range of move, and the infant displays an ability to flex and extend the neck simultaneously.
- Torticollis may be seen in some infants. This is the inclination of the head to ane side of the body as a result of the muscular contractions along that side of the neck. It is expected to subside over time.
Yard. Breast
- Chest anteroposterior and lateral diameters should be about equal at nascency, giving the infant's chest a circular appearance.
- The chest measures approximately 30-33cm at nascence.
- Respirations should exist diaphragmatic, where the chest and abdomen should ascension and autumn synchronously. A seesaw blueprint of respirations may signal distress and needs immediate interventions.
- Bronchial sounds should be heard upon auscultation.
- Nipples should be prominent and appear to be slightly edematous. Some infants may accept milky secretions on their nipples when expressed. This is termed as witch's milk and is a normal occurrence due to the influence of maternal hormones in utero.
H. Skin
- The infant'southward skin should appear to be pink-cherry-red among light-skinned newborns and pinkish-brown or pink-yellow amidst dark-skinned infants.
- Vernix caseosa , a cheesy-white substance covering the infant's trunk that protects the skin inside the uterus, may be seen more than prominent forth the skin folds. This may be more pronounced among preterm infants and less axiomatic for infants above 42 weeks of gestation.
- Lanugo , fine downy pilus, may be seen more prominent on the infant's back, along the arms and the legs. This is normal and the baby sheds this over time.
- White sebaceous glands called milia may also be seen to appear on areas of the face up such as the nose, brow and chin. These glands may reduce in size and disappear in the outset few weeks of life.
- Post mature newborns may appear to take dry skin and peeling is unremarkably seen among them.
- Premature newborns may present with plethoric coloring. This is characterized by dark cerise coloration of some areas of the skin and maybe secondary to over oxygenation upon commitment. This coloring will resolve after a few weeks.
- Cyanosis may be noted in the first few hours afterwards nativity, specifically acrocyanosis or peripheral cyanosis of the hands and feet. This unremarkably resolves during the get-go 2 weeks of life.
- Good pare turgor should exist noted, as this indicates hydration status of the infant. Cess of skin turgor may be done over the belly.
- Some infants may also be seen with various birthmarks, which may be a normal cess finding.
- Harlequin Sign , a deep pink or red coloration seen on one side of the body while the other side may remain normal in color or turn stake, may be observed. This is due to the shunting of the blood from 1 side of the trunk to the dependent portion and may indicate a cardiac trouble or a septic condition. Presence of this sign needs to be reported immediately.
I. Abdomen
- The umbilical cord of the infant should accept 3 vessels: i vein and 2 arteries. Any finding that is not inside this range should be reported to the physician immediately equally it may betoken intrauterine fetal growth restriction (IUGR), genetic abnormalities or congenital center an0malies.
- The cord should exist assessed for bleeding and whatever odor to make up one's mind presence of infections. Infected string should be treated with antibiotics equally prescribed.
- Assess for presence of abdominal amplification, noting for presence of masses, obstacle or hernia. Written report these findings to the physician right abroad.
- Bowel sounds should be present within the offset hour later nativity.
- Infant should besides be able to pass the meconium or the commencement stool within the beginning 24 hours of extrauterine life.
J. Genitals
- For female infants:
- Labia may initially appear to be swollen and the clitoris is enlarged.
- Thick, white mucus drainage may be seen and is a normal finding.
- Blood-tinged mucus, also called pseudomenstruation, may exist seen among infants. This is due to the withdrawal of the maternal estrogen upon delivery. It is a normal finding.
- In some infants, a hymen tag may be visible.
- For male infants:
- The prepuce or the foreskin covers the glans penis.
- The scrotum may also appear to be edematous and testes may retract when the infant is exposed to colder temperatures.
- Some infants may take 1 or both testes partially descended within the beginning few weeks of life, while some may have one of the testes undescended.
J. Spine and Extremities
Nursing Priorities in Caring for Newborn Infants
The newborn infant and the mother are treated as individual patients later commitment and must receive individualized care. Priority of caring for the infant focuses on facilitating his adaptation to extrauterine life, maintaining body temperature within normal ranges, preventing whatsoever complications related to adjustment to the outside environment, and ensuring that the family unit tin can care for the infant finer.
In this regard, the nurse must include the family in planning care for the kid after discharge and impart with them information that would help maintain fetal well-existence. The post-obit nursing diagnoses and care goals may be included in the firsthand care of the newborn.
Newborn Nursing Diagnosis
- Risk for Dumb Gas Exchange
- Hazard for Altered Trunk Temperature
- Ineffective Thermoregulation
1. Adventure for Impaired Gas Exchange
Adventure for impaired gas exchange related to: (the related factors may include but are non limited to: antepartal stress, excessive production of mucus in the airways, stress due to cold environment, improper suctioning of secretions; physical deformities in the airway).
Goal of care: The babe is expected to be complimentary from signs of respiratory distress.
Nursing Interventions:
- Make up one's mind the APGAR Score on the first and fifth minutes of life and record to help determine if at that place is a need for oxygen resuscitation measures.
- Determine if there are any other prenatal conditions or complications which may contribute to infant respiratory distress and report to the physician immediately and then that proper steps may be taken to ensure that the infant would not suffer from further complications.
- Clear the airway from secretions, ensuring to utilise gentle suctioning to prevent damage to airway passages.
- Monitor the apical pulse of the infant during suctioning considering suctioning may stimulate the vagal nerve and cause bradycardia. If the babe becomes bradycardic, finish the suction and report to the pediatrician.
- Ensure that the infant is dry and swaddled comfortably. If the infant is roomed in, encourage the family to concur him or place the babe under a warmer to help decrease the effects of common cold stress on him.
- Promote postural drainage past placing the babe in a modified Trendelenburg position at an angle of 10 degrees to help drain fungus from the airway through gravity.
ii. Chance for Altered Body Temperature
Risk for contradistinct body temperature related to: (choose 1 or more from the following, or signal risk factor identified upon assessment: inability of the infant to have chills, imbalance in body surface expanse compared to infant weight, decreased amounts of subcutaneous fats, thinner epidermal layer, immature thermoregulation).
Goal of intendance: The babe would be free from signs of cold stress; the infant would exist able to manifest improve thermoregulation.
Nursing Interventions:
- Assess for the presence of fetal distress or hypoxia since this is normally seen upon infants who experience heat loss due to evaporation and conduction.
- Ensure that the head of the baby is dry and he is wrapped in a warm blanket.
- Ensure that the child does not come in contact with cold objects and drafts such as air from the Air conditioning unit of measurement, cold stethoscope and exposing a body function unnecessarily.
- Decide the range of temperature that can be considered ambient. Minimize the number of airflows and if necessary, limit the use of air conditioning units since a colder surround may increase the oxygen consumption of the babe.
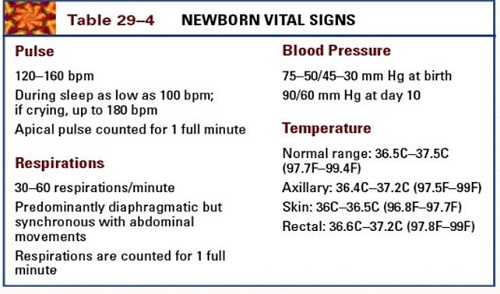
- Maintain trunk temperature within the normal range.
iii. Ineffective Thermoregulation
Ineffective thermoregulation related to exposure to typhoon and cold environs secondary to being undressed/swaddled as evidenced by neonatal temperature below the normal range, increased respirations and heart rate.
Goal of care: The infant's body temperature would be returned and maintained within the normal range.
Nursing Interventions:
- Maintain a neutral thermal environment to determine if the infant'south change in body temperature is caused by the immediate environment or due to other causes.
- Monitor the infant's vital signs oftentimes to determine changes that may warrant immediate intervention.
- Avert exposing infants to drafts, keeping them away from air-conditioning units and doorways. This intervention would assist keep a stable temperature effectually the infant, reducing the run a risk for further bug in thermoregulation.
- Dress or swaddle the infant in warm wear, ensuring that at that place are besides coverings on the caput and extremities to help keep warm and avoid cold.
- Place the baby under bili-light if needed, taking intendance to cover the eyes, genitals and other delicate areas of the trunk to add more warmth and to aid maintain a temperature within normal range.
- Encourage the mother and other family unit members to hold the infant when needed to help maintain temperatures inside the normal range since their trunk warmth can likewise contribute to warming the infant.
References
- Butkus, S. C. (2015).Maternal-neonatal nursing made incredibly easy! Third edition. Philadelphia, [Pa.]: Wolters Kluwer.
- De Sevo, Chiliad. (2016).Maternal and Newborn Success (third ed.). FA Davis Company.
- Flagg. (2017).Maternal and child wellness nursing (eighth ed.). Lippincott Williams and Wilkins.
- Hedstrom, A. B., Gove, North. Eastward., Mayock, D. E., & Batra, 1000. (2018). Performance of the Silverman Andersen Respiratory Severity Score in predicting PCO2 and respiratory back up in newborns: a prospective cohort study.Journal of perinatology : official journal of the California Perinatal Clan,38(5), 505–511. https://doi.org/10.1038/s41372-018-0049-three
- Perry, S. Eastward., Hockenberry, M. J., Lowdermilk, D. L., Wilson, D., Alden, G. R., & Cashion, Thou. C. (2017).Maternal kid nursing intendance (6th ed.). Mosby.
- Pillitteri, A. (2014).Maternal & kid wellness nursing: Care of the childbearing & childrearing family. Lippincott Williams and Wilkins. Wolters-Kluwer.
Source: https://rnspeak.com/newborn-nursing-diagnosis/
0 Response to "Out of the Mouth of Infants and Nursing Babies"
Post a Comment